Lexan Compete
Intelligent Provider Rate Analysis for the Modern Insurer
Date: June 25, 2025
Today's Strategic Conversation
A collaborative discussion on the future of provider rate negotiations
- Understanding the Evolving Provider Rate Landscape in 2025
- The Hidden Costs & Liabilities of Current Rate Analysis Methods
- A New Framework for Data-Driven Rate Negotiations
- How Lexan Compete Powers This New Framework
- The Partnership Path to Implementation & ROI
Navigating Unprecedented Headwinds in Provider Rate Negotiations
Escalating Medical Costs
Provider rates increasing faster than premium growth
Transparency Mandates
New regulations requiring rate transparency
Competitive Rate Pressure
Members demanding competitive provider rates
Data Processing Complexity
Massive transparency datasets requiring sophisticated analysis
Provider Negotiation Challenges
Limited market intelligence for effective negotiations
The Critical Reframe
But what if the greatest challenge isn't the transparency requirements themselves, but your ability to turn this data into competitive advantage?
Most insurers view transparency in coverage data as a compliance burden. Our analysis shows it's actually a strategic intelligence goldmine. Every transparency file published by competitors isn't just regulatory compliance—it's revealing their exact provider rate strategies, network gaps, and negotiation patterns. The insurers who can process and analyze this data fastest will gain unprecedented competitive intelligence.
The Known Problem
Compliance burden and data processing challenges
The Hidden Opportunity
Competitive intelligence and strategic advantage through data mastery
The Unseen Costs of Competitive Blindness
How limited rate intelligence creates a vicious cycle that erodes profitability
Negotiating provider rates without competitive benchmarks
Providers leverage information asymmetry against you
Higher medical costs and reduced margins
Higher costs force higher premiums or reduced profitability
Loss of market share to competitors with better rates
You're Not Alone: The Entire Industry Faces a Data Processing Gap
The Transparency Challenge
89% of insurers struggle to process and analyze transparency in coverage data effectively, despite its strategic value.
The Competitive Threat
67% of health plans report that competitors with better rate intelligence are winning more broker partnerships.
The Resource Barrier
73% of insurers cite 'data processing capabilities' as their primary barrier to leveraging transparency data for competitive advantage.
The Annual Cost of Rate Intelligence Blindness
What Is the Annual Cost of Inaction for [Prospect Company]?
The Story of a Provider Negotiation: A Broken Process
This is Sarah, a senior network manager with 8 years of experience. She's preparing for a critical negotiation with a major hospital system that's demanding a 12% rate increase. Her day is spent manually gathering scattered rate data from internal systems, searching through competitor websites for limited public information, and relying on outdated market surveys. The hospital comes to the table with sophisticated rate benchmarking data while Sarah operates with limited intelligence. The negotiation takes months, and ultimately, she accepts a 9% increase—far above what competitive data would have supported.
"I know we're overpaying, but I don't have the data to prove it."
The Ripple Effect: How Rate Intelligence Gaps Destroy Broker Relationships
— Regional Broker Managing $50M+ in Annual Premiums
The Real Cost
This single broker relationship represents $50M in annual premiums. Without competitive rate intelligence, you're not just overpaying providers—you're losing entire market segments to better-informed competitors.
The Path to Rate Intelligence Leadership
From reactive negotiations to proactive market intelligence
The Old Way
- Manual rate gathering
- Limited market intelligence
- Reactive negotiations
- Provider information advantage
- Gut-feeling pricing decisions
The New Way
- Automated data processing
- Comprehensive market intelligence
- Strategic negotiation planning
- Information advantage over providers
- Data-driven rate optimization
The Framework for Rate Intelligence Mastery
Built on three foundational pillars
Massive Data Processing
Automated ingestion and analysis of transparency in coverage files from hundreds of insurers, processing terabytes of rate data daily.
Intelligent Rate Analytics
AI-powered analysis that identifies rate patterns, competitive gaps, and negotiation opportunities across provider networks.
Actionable Market Intelligence
Real-time dashboards and reports that provide specific, actionable insights for provider negotiations and network strategy.
The Story of a Provider Negotiation, Reimagined
This is Sarah again. The same hospital system demands a 12% rate increase. But now, with Lexan Compete, Sarah opens her dashboard and instantly sees that this provider's rates are already 15% above market average across 12 competitor plans. She identifies three specific procedure codes where the hospital is significantly overpricing compared to similar facilities. Armed with this intelligence, Sarah counter-proposes a 3% rate reduction. The negotiation concludes in two weeks with a 2% rate decrease. The hospital respects her data-driven approach.
"I came to the table with better data than they had. That changed everything."
Lexan Compete
The Provider Rate Intelligence Platform for Enterprise Insurance
We provide a secure, AI-powered platform that processes transparency in coverage data from hundreds of insurers, delivering actionable provider rate intelligence that enables carriers to optimize network costs, strengthen negotiating positions, and gain competitive advantage in rate negotiations.
A Simple, Three-Step Process to Transform Your Rate Intelligence
1. Ingest & Process
Our data lake continuously ingests and processes transparency files from 500+ insurers, handling terabytes of rate data with sophisticated ETL pipelines.
2. Analyze & Benchmark
AI algorithms analyze rate patterns, identify competitive gaps, and benchmark your rates against market standards across procedure codes and provider types.
3. Deliver & Act
Intuitive dashboards deliver specific negotiation insights, rate optimization opportunities, and competitive intelligence reports tailored to your network strategy.
Purpose-Built for Insurance Rate Intelligence
🏥 Insurance-Specific Processing
Unlike generic data platforms, our algorithms understand insurance rate structures, provider hierarchies, and negotiation patterns specific to health plan operations.
⚡ Massive Scale Processing
Our data lake architecture processes 50+ TB of transparency data monthly, handling the complexity that makes this analysis impossible with traditional tools.
🎯 Actionable Intelligence
Beyond data visualization, we provide specific negotiation recommendations, rate optimization targets, and competitive positioning insights.
🔒 Enterprise Security
Built for healthcare data with SOC 2, HIPAA compliance, and enterprise-grade security that meets the strictest insurance industry requirements.
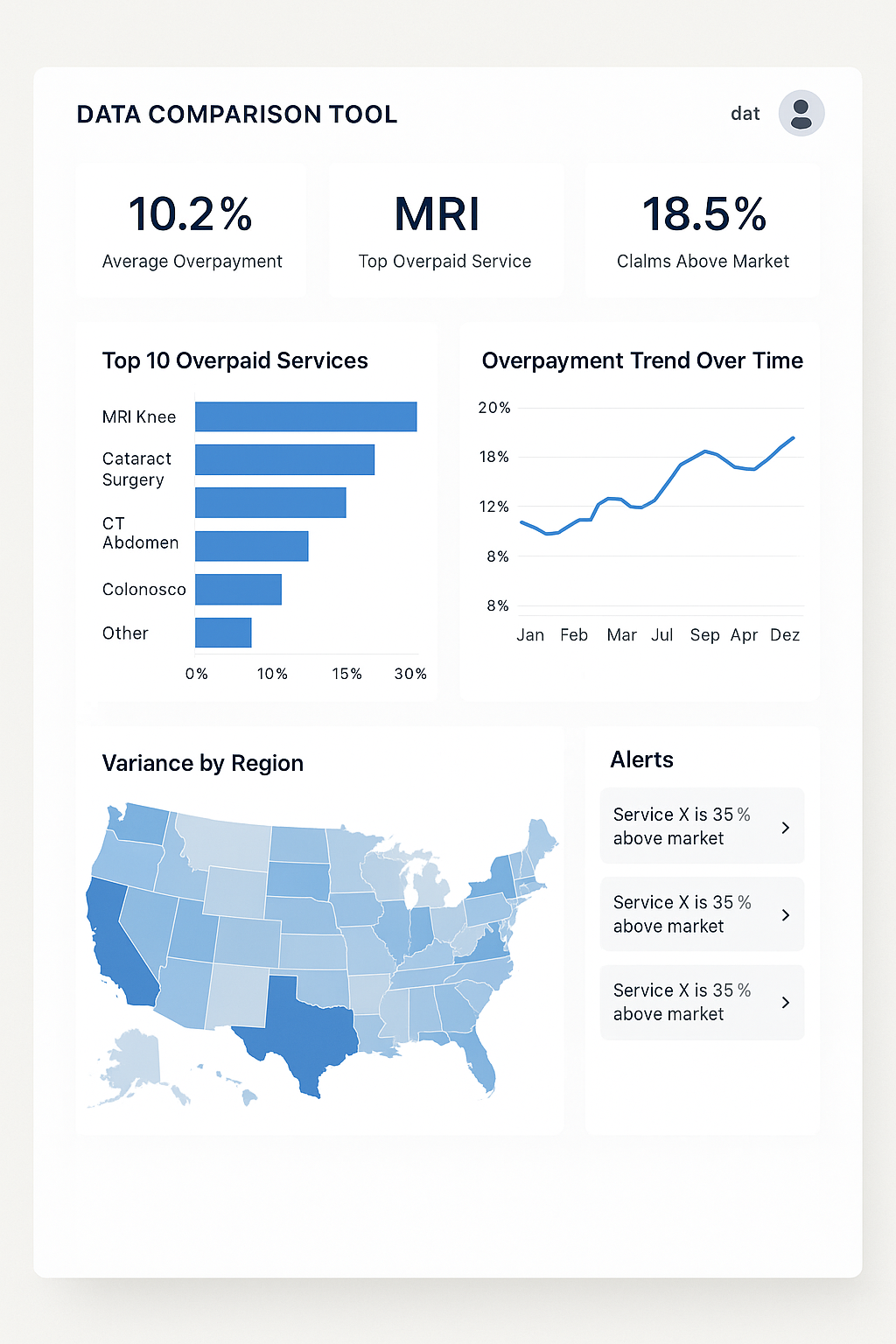
See Rate Intelligence in Action
Competitive Rate Analysis
Instantly compare your rates against 15+ competitors for any provider or procedure code.
Negotiation Preparation
AI-powered insights identify specific leverage points and rate adjustment opportunities.
Market Position Dashboard
Real-time view of your competitive position across your entire provider network.
Proven Results and Tangible Impact
Pilot Program Results
$12MAnnual savings identified in a 6-month pilot with a regional health plan covering 500K members through optimized provider rate negotiations.
Client Testimonial
— VP of Network Management, Regional Health Plan
Platform Performance
500+Insurers analyzed, 50TB+ data processed monthly, 99.9% platform uptime, 100% client retention rate.
A Phased, Low-Risk Path to Rate Intelligence Mastery
Phase 1: Days 1-30
Discovery & Setup
Our team works with yours to identify priority provider relationships and configure initial rate analysis parameters.
Phase 2: Days 31-60
Intelligence & Insights
Platform goes live with your first competitive intelligence reports and negotiation recommendations.
Phase 3: Days 61-90
Scale & Optimize
Expand analysis to full network with advanced analytics and custom reporting for your specific market needs.
Partnership Support Includes:
- ✓ Dedicated Customer Success Manager
- ✓ Custom Rate Analysis Training
- ✓ Ongoing Market Intelligence Updates
- ✓ Advanced Analytics Consulting
Security and Compliance are at the Core of Our Platform
Enterprise-Grade Security for Healthcare Data
A Team of Insurance and 15+ Years Technology Veterans
Bhuvanesh Ram M
CEO & Co-Founder
15+ years technology experience with the past 6 years as CTO building various AI and ML products
Goutham Deepak A
CTO & Co-Founder
15+ years technology experience with the past 10 years as Lead infra and data architect
Our Vision: To Build the Intelligence Layer for Healthcare Economics
Now
Rate Intelligence Foundation
- Provider Rate Analysis
- Competitive Benchmarking
- Negotiation Intelligence
Next 12-18 Months
Advanced Analytics
- Predictive Rate Modeling
- Network Optimization AI
- Risk-Adjusted Benchmarks
Future 18+ Months
Market Intelligence Platform
- Real-time Market Dynamics
- Automated Negotiation Insights
- Regulatory Impact Analysis
A Simple Model for a Clear Return on Investment
Transparent Pricing
Simple, usage-based pricing starting at $50K annually for regional plans, scaling with covered lives and data complexity.
No hidden fees, no long-term contracts
Proven ROI
Average return on investment. By addressing the $65-115M Annual Cost of Rate Intelligence Blindness, clients typically see 10-20x ROI within the first year.
Typical Client Results
3-7% reduction in provider network costs, 15-25% improvement in negotiation outcomes, 6-9 month payback period
Let's Build Your Business Case for Rate Intelligence Leadership
Proposed Next Step: Rate Intelligence Assessment
Our proposed next step is a 2-week, no-cost Rate Intelligence Assessment. We will analyze a sample of your current provider rates against comprehensive market benchmarks under a strict NDA. We will then provide a custom report detailing the specific savings opportunities, competitive gaps, and negotiation advantages that [Prospect Company] can expect to achieve.
This provides you with a data-driven business case to share internally before making any commitment.
What You'll Receive:
- ✓ Competitive rate analysis for top 20 providers
- ✓ Specific savings opportunities identified
- ✓ Custom ROI projections for your market
- ✓ Implementation roadmap and timeline
Thank You
Questions & Discussion
Ready to Transform Your Rate Intelligence?
🌐 www.lexan.health